Severe Leg Trauma: a journey.
Great thanks to the patient who has allowed this blog to be written about his trauma and ongoing recovery, on request his name has been changed, I have chosen to use the name Drew, according to google this is a Greek derived name meaning brave.
On the 11th November 2022, Drew, a Tree surgeon (Aborist) stepped back into his stump grinder in a lapse of concentration. This powerful machine designed for destroying tree stumps caught Drew’s left lower leg to spin and threw him several feet, finding himself on the grass looking down at a horrific open injury where flesh and bone was in complete disarray. Time was of the essence, as Drew’s blood loss was weakening his shouts for help above the ongoing noise of the stump grinder. Fortunately, passing dog walkers heard Drew’s desperate shouts and under Drew’s instruction created a tourniquet from their dog lead preventing an entirely different scenario.
Drew had visited the Waterside Practice for back pain prior to his injury to see our Osteopaths, and due to his own drive to improve his prognosis since having 7 operations to save his leg with no immediate physiotherapy on the cards. I agreed to assess initially for the purpose of his ongoing back complaint, however this quickly developed into rehabilitation for his leg function and associated pain.
Rehab for traumatic injuries is not something that, since graduating as an Osteopath in 2011, I have had any major experience with. There has been an increase in post fracture patients seeking Osteopathic care since the pandemic, which has been something an Osteopath can adapt well to. But not something of this traumatic nature; where bones are missing, others are being regrown and muscles have endured extreme trauma.
Drew presented to me on the 16th June 2023 and told me his story. As an independent business owner, he was working with dangerous machinery most days of the week and at the time of his injury had been working flat out, fatigued and very short staffed. After leaving his home that day telling his wife who was on maternity leave that he was to be home for lunch, instead he was to become an inpatient at Addenbrookes Hospital. Discussions between orthopaedic and plastic surgeons later took place about amputation, or feasibility to save the leg. Drew didn’t get home until a month later.
We started recording and taking images from September, 3 months after Drew first came for assessment. It would have been best to start from day 1 with media however, this was not something that was emotionally appropriate at the time for Drew or had occurred to me as a therapist.
The surgeon’s agreed to save Drew’s leg, a painful process to say the least due to the extent of the trauma. The fibula bone was almost completely destroyed, the tibia bone had a complete fracture top and bottom, pulled out of the leg and with a total of 71mm missing from the superior end. Altogether, there were seven breaks in the tibia and fibula. Muscles were all over the place and all three arteries to the lower leg had also been severely damaged.
See picture below for normal anatomy, the fibula bone is a thinner long bone alongside the long tibia (shin) bone:
Image taken from Kenhub.com
Following 5 operations in November including a skin graft, Drew then had a 6th operation in late February to have a TSF frame fitted to the lower leg in order for new bone growth to take place. A foot plate was then surgically fitted during a 7th operation in April to stop the foot from curving round, this gave the patient a fighting chance of being able to maintain his ankle joint un-fused.
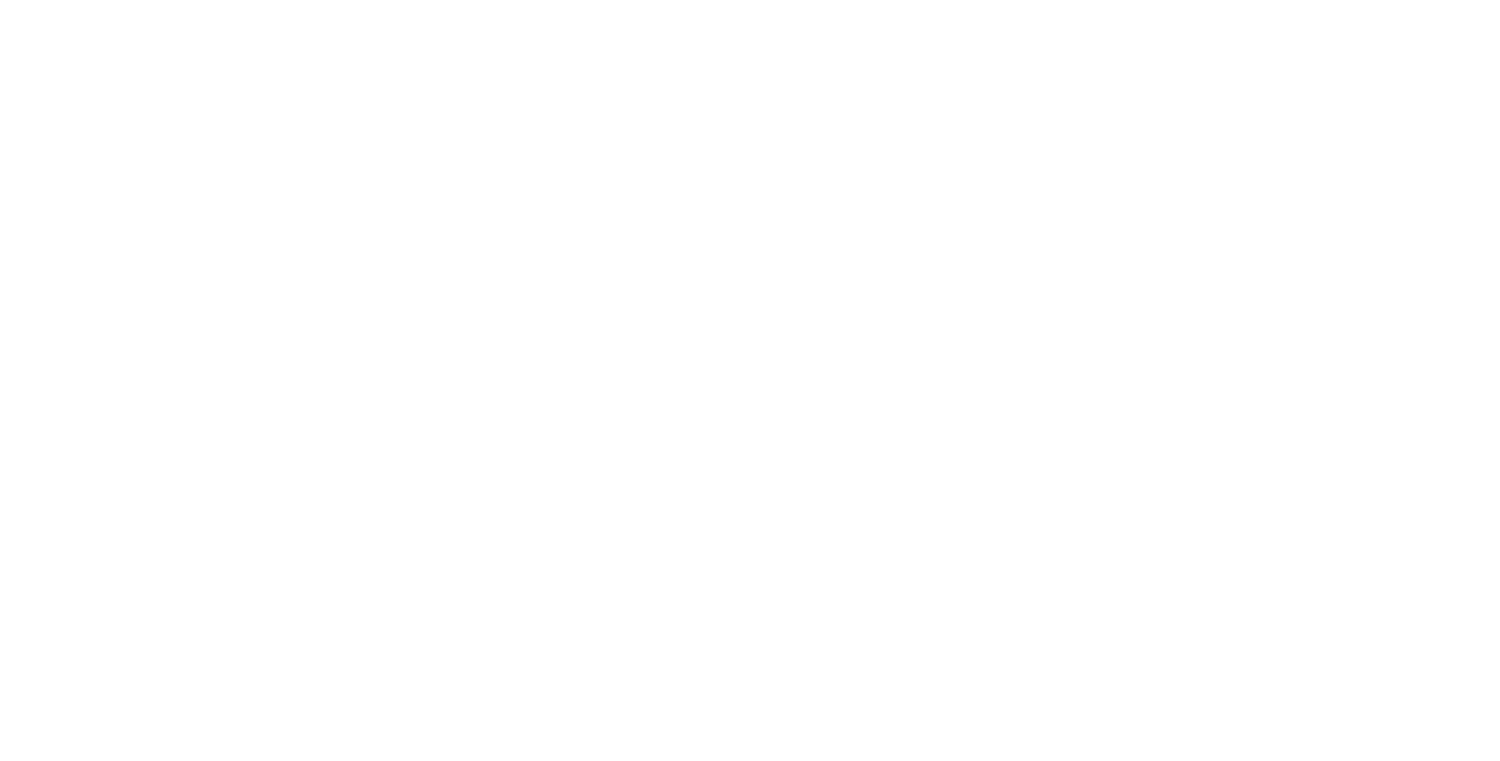
TSF Frame fitted to regrow the tibia bone with foot plate in place.
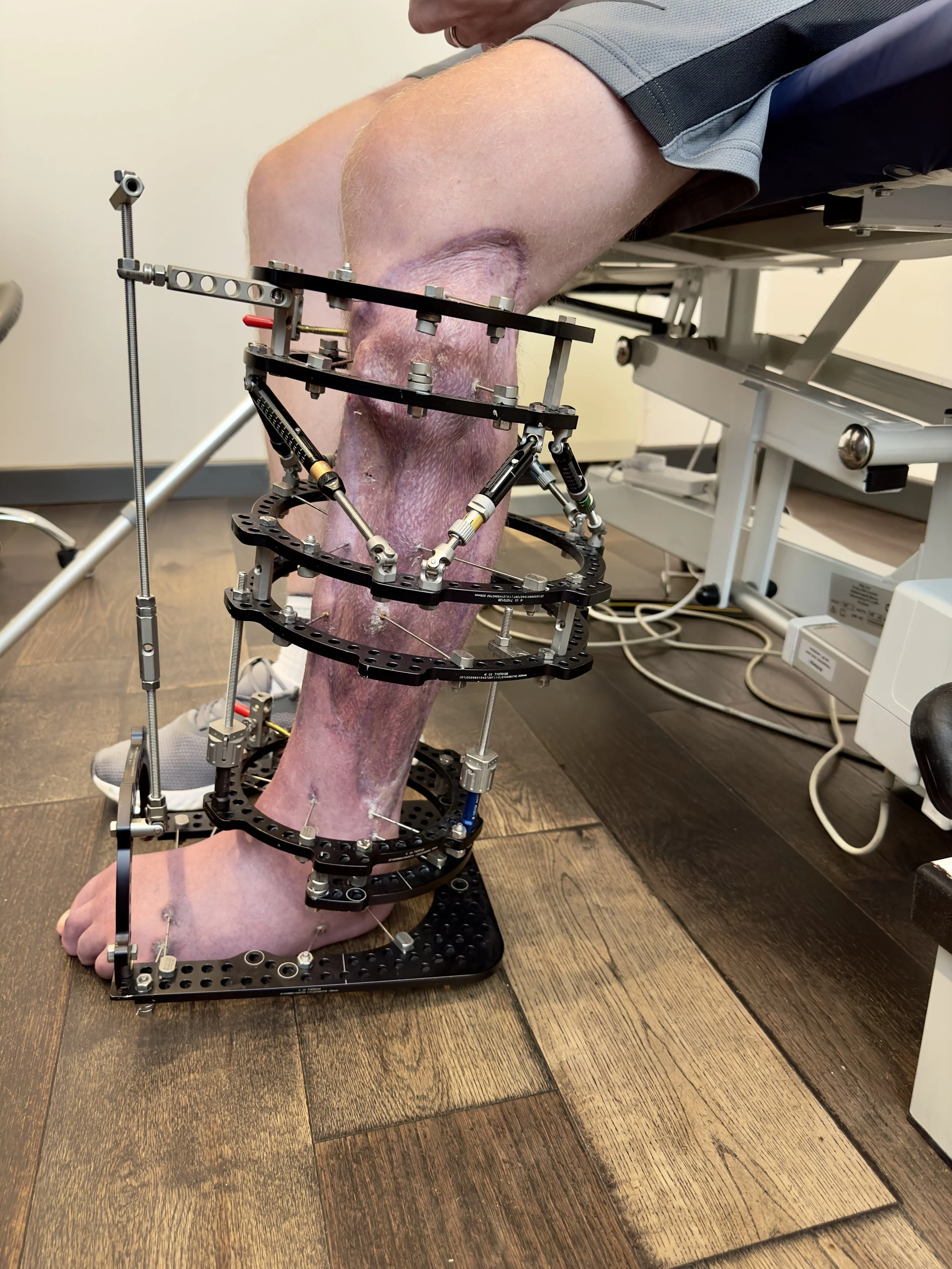
As you can see from the image above, there are multiple pins which are passing through drilled bone. The lower third of the TSF frame, where there is a gap in these pins, is where regrowth of bone has been taking place throughout 2023.
After initially treating Drew’s mid and lower back pain, adapting techniques to allow for the positions that were difficult to be in, we moved onto rehab for the leg. Osteopath’s are trained to look at the structure and function of soft tissues, joints and bones. Every part is worthy of attention when assessing a patients pain.
For Drew, we have had targets, either directly from Drew, his consultant’s feedback and/or my own goals as an Osteopath for purposes of improving biomechanical elements. As we progress and update this blog throughout Drew’s rehabilitation, these will be added to this blog.
Goal One: Curling toes: September 2023
Foot arch shape change, toe curling with visual puckering of the foot sole (top end).
The main reason for the foot plate part of the TSF frame being fitted in April, was that the foot was twisting inwards. If this was to continue, the ankle would have had little chance of maintaining correct position for walking and a fusion of this joint was to take place. Alongside this twisting, the toes were curling underneath the foot and had no independent active movement of their own and a visual skin puckering of the distal plantar foot arch was forming.
Improvement shown in foot posture, photo taken December 2023
Together with a direct manual approach to the joints and soft tissues, at home exercises, Drew’s wife giving daily toe massage and gentle passive stretching, the toes have gradually started to relax and now we are starting to see independent movement of each toe. I know that neither of us have never been quite so excited about seeing toe movement before!
Below is a video taken in October of the progress seen the following month:
Goal two: Ankle Strength
Feedback from Drew’s consultant in September alongside his hesitation to move onto the next stage in the TSF process by removing the foot plate, was contributed by the lack of dorsiflexion through the ankle joint. To progress to the next stage, we started focusing treatment to this goal: improving the talocrural joint mobility and strength.
In order for the ankle joint to dorsiflex (toes towards head) you need the following:
muscular strength and function - anterior compartment lower leg
talocrural (ankle) joint range
Achilles tendon function and tissue quality
As a result of the lower leg trauma, a huge portion of the anterior compartment musculature is now missing, making strength building here to achieve better active dorsiflexion even more of a challenge. If you look back to the second photo of the blog and retake a look at the leg showing the TSF frame and footplate, you can clearly see the outline of the tibia bone due to the lack of fibula and missing soft tissues.
However, with Drew’s home exercises of concentrating his attention to dorsiflexing the hallux (big toe), we started to see twitches in the anterior shin strips of muscles on activation .. hard to say exactly which muscle due to surgery reattachment - could be tibialis anterior. Seeing this gave the foundations for building size and strength for active dorsiflexion musculature, see below!
Drew’s range of talocrural passive motion was also monitored by video at sessions to be able to look back on and compare later on. You can see how rigid the lower leg is, the lack of tissue stretch at the posterior lower leg causes the heel to lift.
This led us onto treatment sessions involving direct work to the Achilles and gastrocnemius soft tissues, we recorded a demo for Drews wife to replicate at home which she did daily. Drew has also now managed to use a tool to self massage the anterior muscles of the lower leg and dorsum of the foot. This all contributes to loosening the soft tissues underneath the rigid TSF to rehab these traumatised soft tissues and eventually helping our goal to regain active function in the future.
Goal Three: Footplate is OFF!!
On 7th February 2024, Drew came into the clinic with a huge grin on his face after having his foot plate removed the day before. Usually to remove the 4 pins going through the foot patients are sedated however, after being told by the consultant that to book this in would be another 2-3 months of waiting - Drew opted for gas and air in the treatment room next door. Drew reported this was not for the faint hearted, especially as by the 4th pin to slide out of the bones (which was no easy task as the ‘olive’ part of the pin, meant to be outside the bone, was partially embedded) Drew was shaking and sweating in anticipation.
The position of the foot was still in a good place, without seeing the foot curling under at this stage. This being the reason the footplate was fitted initially.
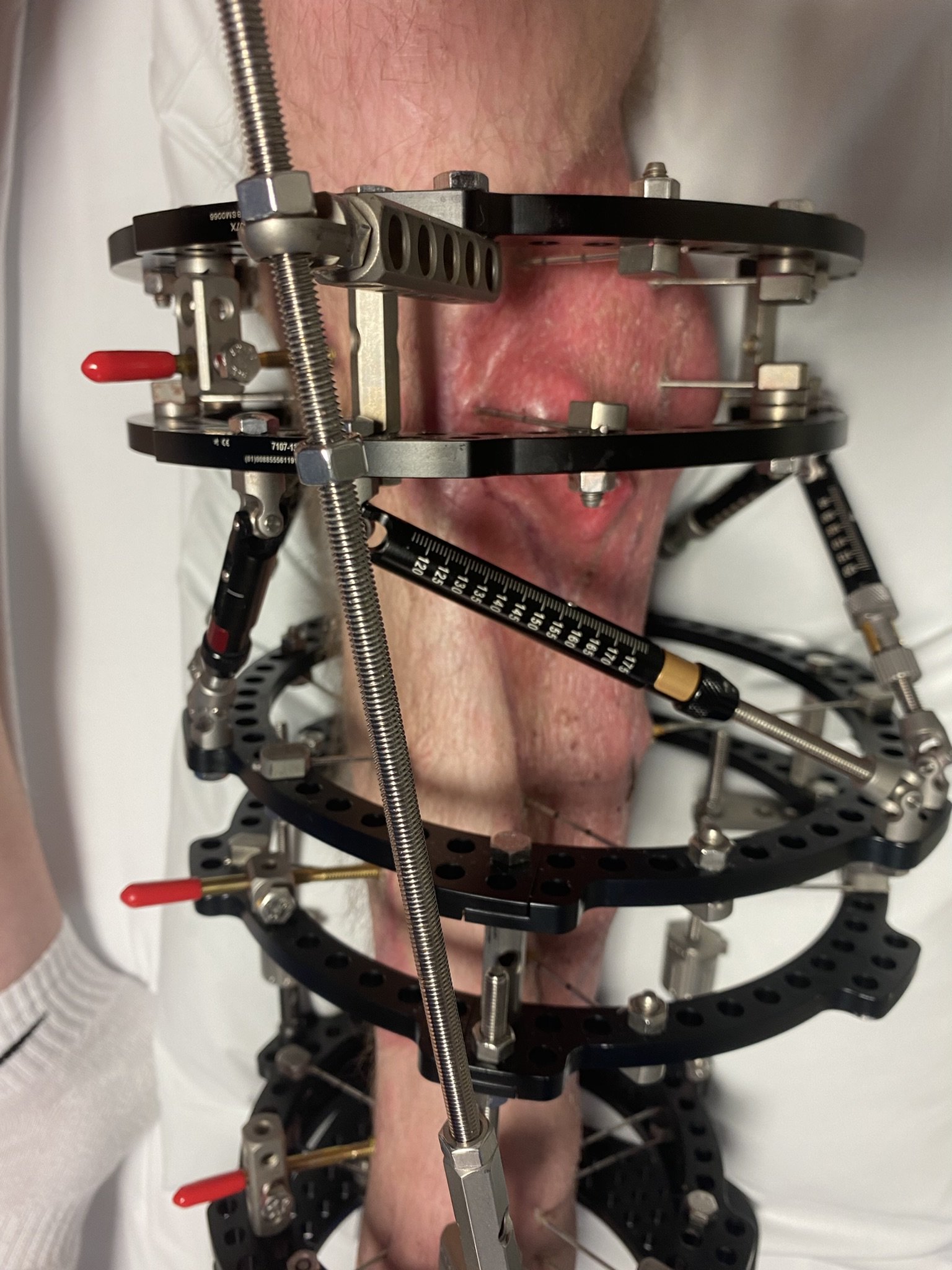
Foot Plate removed 6th Feb 2024
So now the race is on to keep the foot in good alignment and to start weightbearing. The section of bony regrowth in the lower tibia was reported to be looking good on X-rays and now the process of the bone maturing and hardening will be in theory helped with more opportunity to walk. Pins from the TSF now end above the ankle joint, allowing full access to treating the foot anatomy rather than manoeuvring direct treatment around the foot pins - which has not been the easiest of tasks (not complaining though!).
Proprioceptive foot exercises were given after this session engage what muscles remain in the lateral and anterior compartment muscles of the lower leg (the outside/lateral to the calf area), Drew had good activation of these and I’m looking forward to seeing the strength of these progress. He has already made good progress rebuilding bulk in these muscular compartments.
Drew wishes to set a goal of walking more normally on that side, the left hip area has compensated its gait to raise the leg in a straight fashion due to the weight of the frame on the hip and knee. As we still have the bulk of the TSF, I explained to Drew that if I put a couple of kg weight on one leg - my hip would adapt a similar motion. Next session we plan to start looking at the hip musculature, lumbar spine function to help with improving this gait pattern.
So, next goals involve using the foot for walking and keeping good foot alignment. Till the next update!
Goal Four: Foot position and gait
May ‘24 update:
Drew has been working hard at the gym and is now even now able to wear a shoe on his left side, however has some difficulty getting the forefoot comfortably into the end of the shoe due to lack of active toe extension. Although once the shoe is on, ensuring the toes aren’t caught underneath the foot - he actually finds his gait is improved when walking. Perhaps the sensory feedback from the shoe is getting those neurons back to the brain firing!
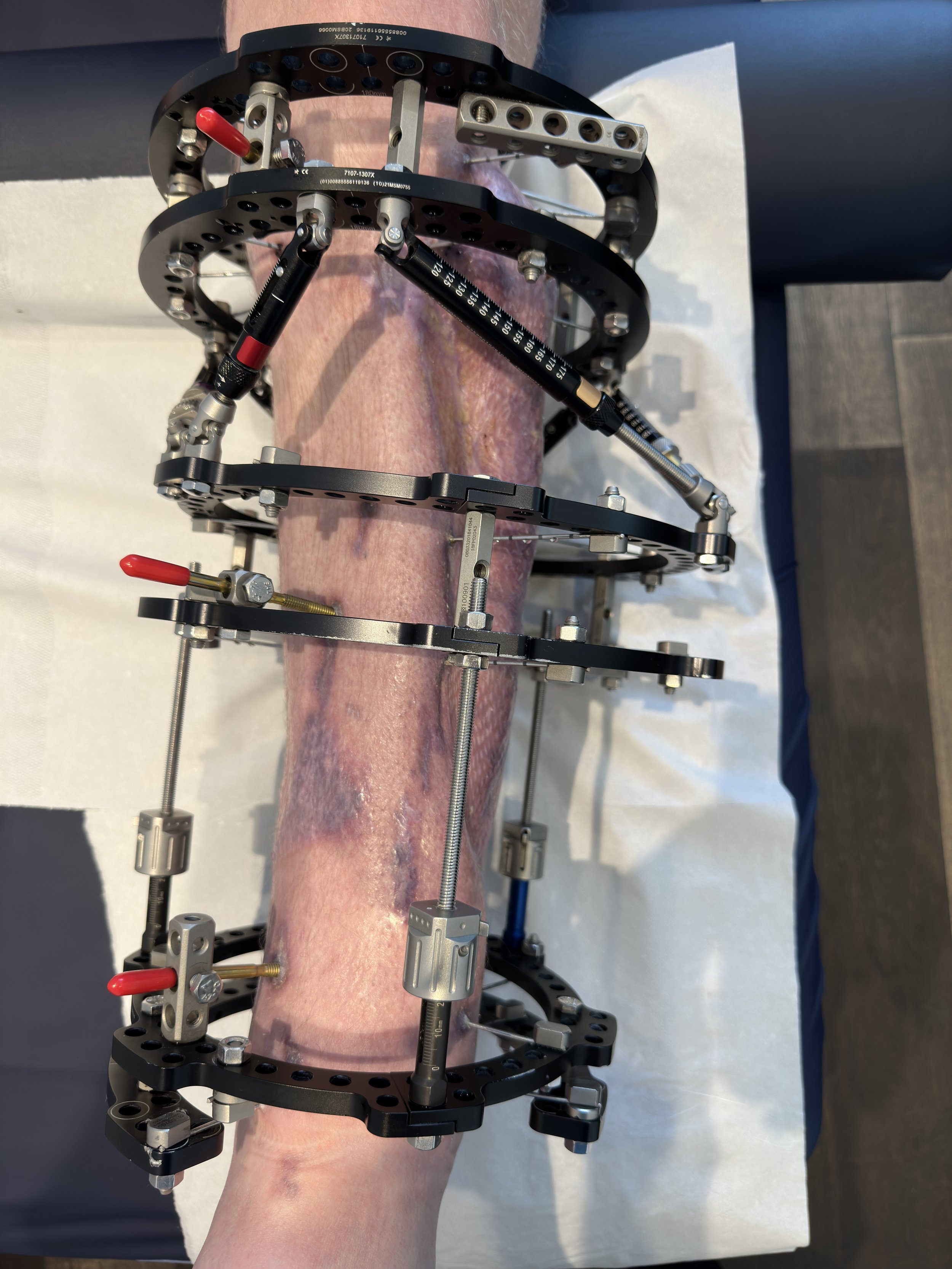
As a result of his hard work walking, at the gym (using the exercise bike now), even mowing the lawn now (one handed!) has gradually built up the anterior compartment muscles of the left shin. See below for comparison pictures May ‘23 to this April ‘24..
If you look at the gap in musculature on the left photo between the shin bone (tibia) and the fibula (outside smaller long bone), then compare this to the photo on the right. You will see it has filled in well where the anterior compartment muscles are located which, usually include; tibialis anterior, extensor hallucis longus, extensor digitorum longus, and fibularis tertius. With the extent of muscular damage to the lower leg on injury knowing exactly which muscles are left can be tricky however, with regular stimulation and loading of this compartment we can now start to show what musculature is remaining.
Drew’s progress is admirable and is now heading towards the 2024 goal of taking the TSF frame off entirely, the main concern being the left foot curling under into pronation and resulting in a surgical fusion. However, to date the foot has maintained a good enough position and is a daily focus with home exercises for Drew.
Current Goal: continue foot gait and walking position.
Next 2024 Goal TSF frame removal!
Goal 4 update August ‘24
Drew is ready and waiting for his TSF Frame to be removed after consultant approval has now been achieved, a major milestone in rehabilitation as Drew has been finding regaining a better gait pattern very challenging with the weight and restriction of the frame still in place.
With regular gym sessions, introducing resistance bands to rebuild the anterior compartment (shin) muscles of the lower leg and a close eye on being kept on the left foot which, is becoming a battle to control the inward (medial) deviation. Drew is well due to start the next stage of rehabilitation, TSF frame-free.
The next stage will be exciting for both Drew and all therapists involved, what a journey it has been so far.